Brigitte Schiller, MD, FACP, FASN, SVP, Medical Officer: Home Therapies, Global Medical Office, Medical Affairs, Fresenius Medical Care
Important progress has been made in the delivery of dialysis. The “one size fits all” approach with standard thrice-weekly in-center hemodialysis shifts toward personalized care, emphasizing quality of life, independence, and symptom management tailored to each person’s clinical and personal needs. Kidney replacement therapy at home is a critical ingredient in this effort.
While kidney transplantation remains the gold standard of end-stage kidney disease (ESKD), most people require dialysis before receiving a transplant. As patients await transplantation, selecting the appropriate dialysis modality is critical.
Person-centered Kidney Replacement Therapy Choice:
Person-centered care requires understanding each person’s clinical needs, personal values and beliefs, hopes for the future, and life circumstances.
Education about all available options of kidney replacement therapy, in-center and home dialysis, often results in patients preferring home dialysis modalities, which offer greater flexibility and independence.
Peritoneal dialysis, provided as continuous ambulatory PD (CAPD), or automated PD (APD), is often the initial choice at the start of dialysis need. People of all ages undergo peritoneal dialysis. In recent years, people older than 65 years are increasingly choosing PD as their modality choice, allowing them to participate in life’s activities (1).
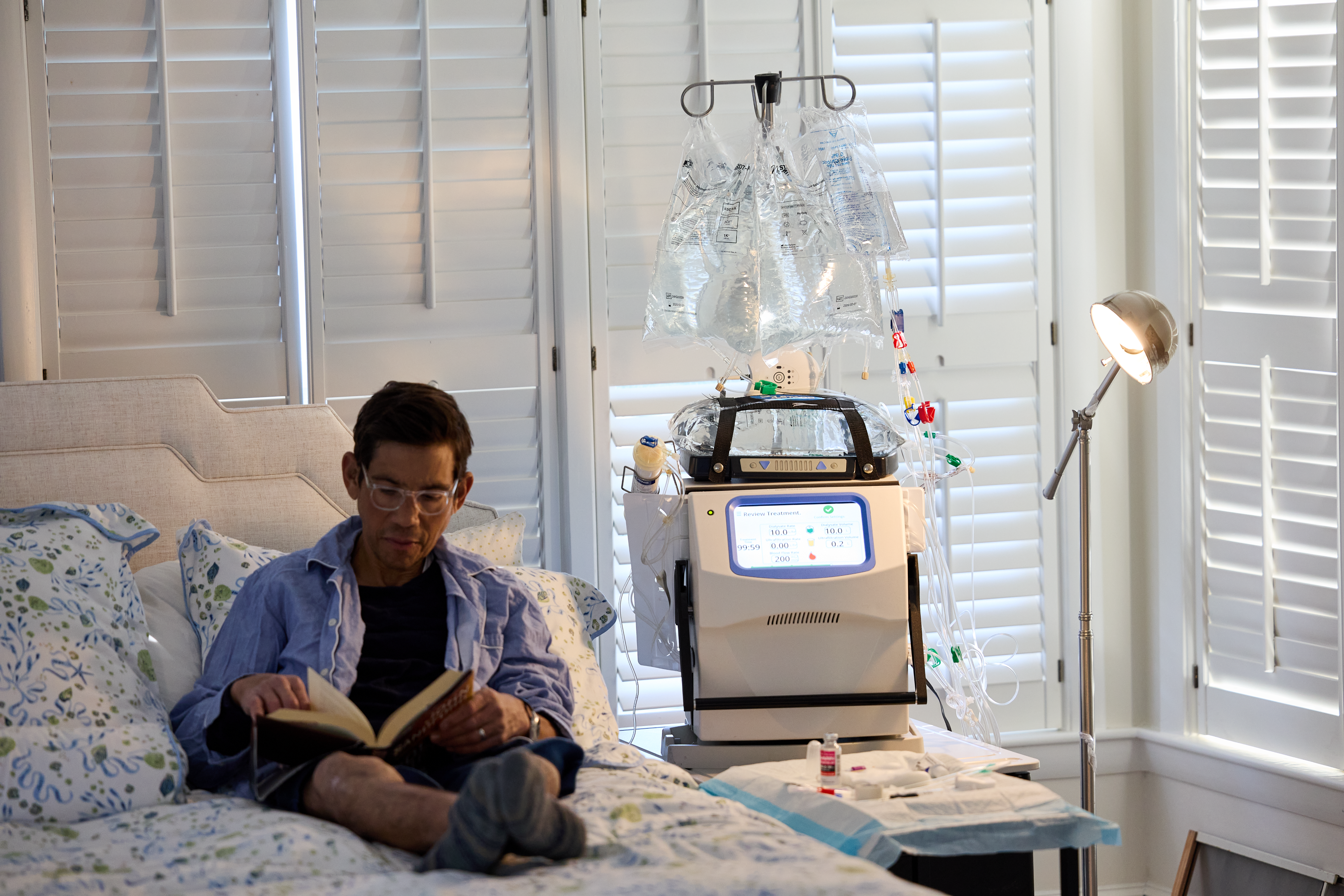
Hemodialysis at home is delivered as more frequent home hemodialysis (HHD) with most people undergoing 4-6 treatments/week (2). Treatment length ranges between 2.5 to more than 6 hours based on individual clinical needs and lifestyle preferences. HHD has been successfully used since the 1960s and 1970s. It re-emerged in the US in the mid-2000s and has quadrupled over the past 20 years (3). Today, more than15,000 people in the US undergo more frequent HHD. Approximately 40% of people choose the therapy within the first year of dialysis, while most people transition later to HHD, with many of them after 5+ years of dialysis. As with PD, increasing number of older patients now choose HHD, reflecting the increased expertise in safely providing home dialysis to older people with other ailments (1).
Patients who choose home dialysis consistently highlight independence, flexibility and the pursuit of normality with time for work, family, friends, socializing and caring, travel and participation in daily life. Benefits of more frequent HHD include improved survival (4-6) reduced cardio-vascular risks (7-9), better sleep quality (10), shortened post dialysis recovery time (11,12) and better overall quality of life (13).
Many patients report satisfaction with their decision to undergo home therapies as it provides them with greater control over their lives.
Nocturnal HHD
Nocturnal HHD, performed overnight while patients sleep, is an appealing option with limited impact on daytime burden with dialysis. The NxStage System One / VersiHD is approved by the FDA for HHD at night with care partner and for daytime dialysis with or without a care partner (solo HHD).
Evidence supporting Nocturnal HHD
Several observational studies conducted in Canada, the US, and internationally have shown survival advantage with nocturnal HHD (14-19). Patients undergoing nocturnal HD have survival comparable to people treated with a cadaver kidney transplant (6). A more recent study in the US confirmed these results in patients undergoing nocturnal HHD for 20 or more hours of therapy during at least 4 sessions per week (20). One contrasting study, the Frequent Hemodialysis Network (FHN) Nocturnal Trial reported worse outcomes in the nocturnal group compared to conventional HHD. However, these findings should be interpreted cautiously due to small sample size and unusually low death rates in the conventional group limiting generalizability of the data (21).
Considering the existing evidence, many nephrologists consider nocturnal hemodialysis with gradual removal of toxins and fluid over a longer treatment time a superior modality which is not often prescribed in the US (22).
Who might consider nocturnal HHD?
- Patients who could benefit from nocturnal HHD include those with cardiovascular health issues, large fluid gains, uncontrolled phosphorus levels, blood pressure drops during dialysis, long recovery times after dialysis.
- Patients who experience burn-out with daytime dialysis might consider taking the therapy out of their daytime and dialyzing while sleeping.
- Patients whose daytime activities and/or the availability of a care partner favor nighttime dialysis.
- Patients who switch from PD to another modality can continue home dialysis at night with this modality choice.
Patients transitioning to nocturnal HHD often report notable improvements in energy and post-dialysis recovery.
Patient Voices: Real World Experiences
Personal Experiences show the potential life-changing benefits of nocturnal HHD:
“We always talk about transplants being the gift of life, but quite frankly, nocturnal home hemodialysis has been my gift of life.”
One patient described their initial transition to nocturnal HHD:
“I started with five-hour treatments in my recliner during the evening, planning not to sleep. But to my surprise, I found I slept during most of the treatment and the needles were stable in place. My confidence grew after several treatments and soon I’ll move to overnight treatments in bed.”
Conclusion:
The positive experiences of many patients with nocturnal HHD motivate ongoing support and awareness of nocturnal HHD as an alternative modality to daytime HHD. Overnight dialysis, when less disruptive to daily routines, improves quality of life. Benefits of outcomes comparable to cadaver kidney transplantation come from observational studies. Safety protocols including securing needles appropriately and including blood detection devices at the needling sites, seek to reduce the risk of serious adverse events, which are very rare (22).
Although nocturnal dialysis still carries burdens, patients often find it less burdensome than other dialysis options.
People undergoing dialysis and considering nocturnal HHD are advised to discuss the option with their nephrologist to ensure safe and individualized person-centered therapy.