By V. Scantlebury, MD, FACS
Chronic kidney disease is associated with phosphate retention due to a decrease in the ability of the kidneys to filter phosphate, especially as your kidney function falls below 25 ml/min. Once you start renal replacement therapy, there is an accumulation of phosphorus that is not removed by dialysis treatments. This occurs because of both decreased filtration and decreased excretion of phosphate in various areas of the kidney.
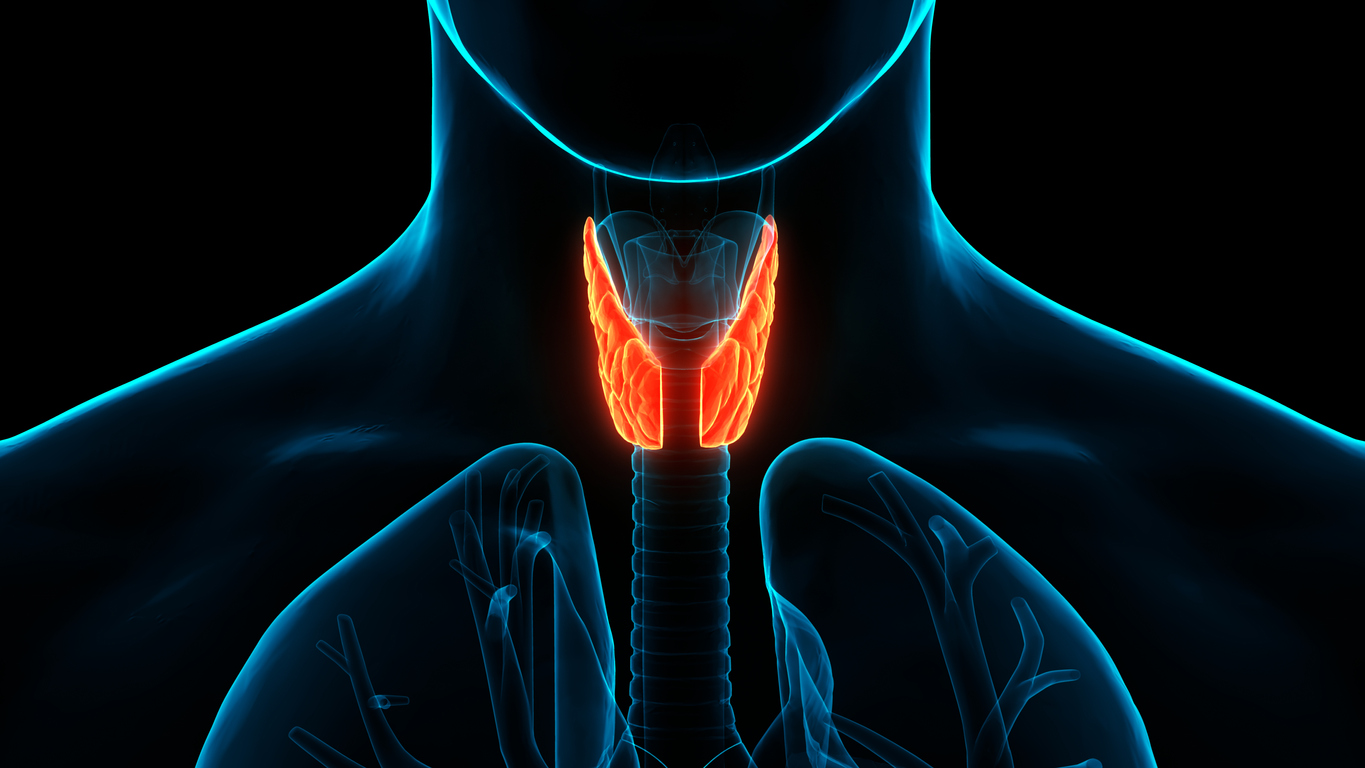
High phosphate levels are a stimulus for hyperparathyroidism: the over secretion of parathyroid hormone (PTH) from the glands. There are usually four parathyroid glands located in the neck, all are in close proximity to the thyroid gland. The parathyroid glands are small, about the size of a grain of rice.
Increased PTH secretion (hyperparathyroidism) results in an imbalance of our normal levels of calcium and phosphorus, and an associated decrease in calcium levels.
Primary hyperparathyroidism occurs when the cause is due to overactivity of the parathyroid glands themselves, such as due to an adenoma of one of the four glands. Removing that adenoma often resolves the issue.
When hyperparathyroidism is due to other causes such as high phosphate levels (hyperphosphatemia), it is referred to as secondary hyperparathyroidism. The treatment here is to restrict phosphorus intake and administer phosphorus binders to decrease the stimulus for more parathyroid hormone secretion. It is also important to measure and keep calcium levels from dropping below normal levels. With high levels of phosphates, the release of PTH will be stimulated by the low calcium levels which are present.
Severe hyperparathyroidism that is unresponsive to medical therapy may result in extremely high levels of parathyroid hormone (>800 pg/ml, with normal level of 65 pg/ml). This is referred to as tertiary hyperparathyroidism, which results from prolonged hyperphosphatemia and hypocalcemia. Once the parathyroid glands have reached this stage, they often no longer respond to normal suppression stimuli, and remain in the overdrive mode, continuously secreting large amounts of PTH hormone. Tertiary hyperparathyroidism is associated with hypercalcemia in the absence of medications such as vitamin D or calcium-containing phosphate binders
These extreme PTH levels can cause such symptoms as
- bone pains due to loss of calcium from bones,
- kidney stones because of too much calcium in your blood
- cardiovascular disease from high calcium level accumulating in blood vessels
- calciphylaxis – calcification of the capillaries in the skin resulting in skin breakdown.
When should patients be referred for parathyroidectomy?
Among dialysis patients, the need for parathyroidectomy is around 7-10 per 1000 patients. The use of agents such as cinacalcet (Sensipar) decreases the risk for hypercalcemia as well as the risk of parathyroidectomy.
Many nephrologists will refer patients once the PTH level reaches 1000 pg/ml even if asymptomatic. This selection can often be reserved for patients less than 65 years of age with few underlying co-morbidities, but not necessarily. However, data has shown that the possible benefits of parathyroidectomy include increased survival, increased bone density and decreased risks of fractures and improved nutrition (1-3).
Since the symptoms attributed to hyperparathyroidism are often seen in dialysis patients (pain, weakness, itching), it can be difficult to separate if the cause is due to high PTH levels. If you have consistent PTH levels over 1,000 pg/nl you might likely be a candidate for parathyroidectomy.
References:
- Improved long-term survival of dialysis patients after near-total parathyroidectomy.Sharma J, Raggi P, Kutner N, Bailey J, Zhang R, Huang Y, Herzog CA, Weber C J Am Coll Surg. 2012 Apr;214(4):400-7; discussion 407-8.
- Survival following parathyroidectomy among United States dialysis patients.Kestenbaum B, Andress DL, Schwartz SM, Gillen DL, Seliger SL, Jadav PR, Sherrard DJ, Stehman-Breen C Kidney Int. 2004;66(5):2010.
- Rodríguez-Ortiz ME, Pendón-Ruiz de Mier MV, Rodríguez M. Parathyroidectomy in dialysis patients: Indications, methods, and consequences. Semin Dial. 2019 Sep;32(5):444-451. doi: 10.1111/sdi.12772. Epub 2019 Jan 17. PMID: 30656752.
This summary was completed by Dr. V. Scantlebury and does not summarize all the major points of the article, Refractory hyperparathyroidism and indications for parathyroidectomy in adult dialysis patients, authored by L Darryl Quarles, MD, Robert Cronin MD, Michael Berkoben MD. Only some highlights are covered here. For the entire article, please visit https://www.uptodate.com/contents/refractory-hyperparathyroidism-and-indications-for-parathyroidectomy-in-adult-dialysis-patients/contributors