By Dr. Linda Gromko, MD, Guest Blogger
Hi my name is Dr. Linda Gromko and I am a Seattle family practice physician who assisted my husband Steve Williams with both hemodialysis and peritoneal dialysis for three-and-a-half years before his death in April 2011. In coordination with interior designer Jane C. McClure, I wrote Arranging Your Life When Dialysis Comes Home: “The Underwear Factor’ and two other books about my family’s experience with ESRD.
Last month, I discussed the advantages of doing dialysis at home. There’s no doubt that home dialysis – both hemodialysis and peritoneal dialysis – offer the opportunity for more personal flexibility and control. But it isn’t for everyone. If you’ve already said, “There’s no way on earth I would ever even try it,” that’s fine. In-center dialysis has its advantages, too.
But, if we’ve sparked your curiosity, read on. I’ve listed four important requirements for successful home dialysis below:
Requirement #1: A Team that Works Well Together
Steve and I shared a mutual commitment in doing home dialysis. Our goal was to help him live as well as possible until he could get a transplanted kidney. Later, after he had a transplant and an unfortunate outcome, our goal was “simply” to help him live as long and as well as possible.
We established an important ground rule early in the process: there would be no arguing while dialysis was being done. It simply felt too threatening for both of us. I would take Steve’s criticisms way too personally, and there were times when he felt too vulnerable (those are big needles, after all). We learned to remind each other that we were on the same team, take a breath, and work through the problem.
Requirement #2: The Ability to Read and Follow Instructions
Consistency – even to the point of rigidity – is important. At the Northwest Kidney Centers where Steve and I trained, home dialysis was taught as a team endeavor. With our training manuals in hand, Steve would read a single point of instruction, and I would follow it. (I remember him saying more than once, “Don’t freelance here, Linda Jo. You’re getting ahead!”) Staying on task will keep you out of trouble most of the time.
Requirement #3: Adequate Manual Dexterity and Physical Strength
Home hemodialysis requires the ability to attach needles to syringes, draw up saline and Heparin into syringes, and connect plastic tubing together. You must be able to tear tape for securing dialysis hoses, and to insert a “priming spike” into a liter of IV fluid. This might not be possible if your hands are arthritic or painful.
In our case (not applicable to all home dialysis machines), we had to lift 5 or 6 five-liter bags overhead and onto an IV pole before starting each treatment. Each bag weighed ten pounds. Bags had to be removed from cardboard boxes, and removed from their plastic outer-wraps.I would often task our daughter Brita with hanging the bags, and taking care of the cardboard and plastic recycling.
Requirement #4: The Ability to Function Under Pressure
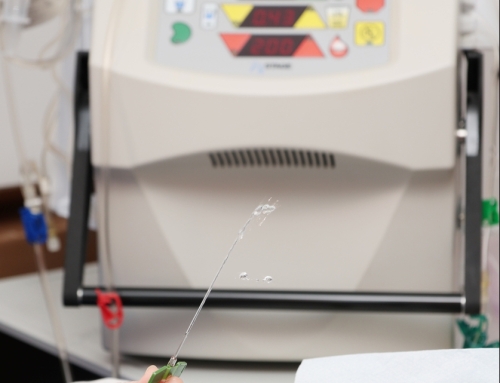
Everyone who does dialysis treatments, whether at home or in a hospital or center, will sometimes experience alarms from the machine that signal something is wrong. Some of the alarms are merely annoying, but others signal a problem that must be fixed immediately.
Training teaches us how to manage these alarms. Alarms are signaled with a bell, and with a visible number lighting up on the machine: yellow alerting us to a concern, and red for deeper trouble. We learned quickly to look up the number being displayed in our manual. The manual would then give us simple steps for immediate troubleshooting.
There were two “hotlines” available for immediate telephone support: one from the nurses at the home dialysis training unit, and the other a technical support line from the company that manufactures the machines. We learned to place a label with these important phone numbers on the machine itself, and to have a phone at hand at all times. We found that we could troubleshoot most problems on our own. But now and again, you will likely call one of the support lines.
I remember one hotline operator asking, “What state are you calling from?” My reply, “From the state of confusion!”
If you know yourself well enough to know that you would panic under such pressure, this really may not be the route for you! But people of all backgrounds and abilities have mastered the skills required for home hemodialysis. It is definitely learnable – and the training and backup support are extraordinary!
What about Home Peritoneal Dialysis?
Steve and I did peritoneal dialysis after three years of hemodialysis. We found it to be much easier. So if this is an option in your situation, it’s definitely worth considering.
The training is shorter: one week versus 4-6 weeks for hemodialysis; the menu of potential problems is less complex. You, too, must have adequate manual dexterity to connect branching bags to your access port in your belly, or to connect to your automatic overnight cycler. You must use the proper “no-touch” technique to prevent infection. You must have the discipline to “get in” all the treatments you need – and to do treatments every single day.
Again, though, excellent training and backup support are available from your dialysis training staff. These are the people who will lovingly guide you through the process and help you every step of the way.
©Linda Gromko, MD